- +91 99202 00400 / +91 22 4113 6565
- contact@neurogen.in
Disclaimer: At NeuroGen BSI, autologous bone marrow tissue, after minimal manipulation, is grafted by medical practioners as part of routine procedure within the hospital in the same surgical sitting. According to the directives of the Ministry of Health and Family Welfare issued under section 33P of the Drugs and Cosmetics Act,1940 this procedure does not involve use of stem cells/ stem cell derived product.
Stroke is a condition in which there is a sudden interruption of the blood supply to the brain, thus, resulting in damage to the brain tissue, as this event cuts off its supply of oxygen and nutrients. This causes the brain cells to die within minutes leading to very serious clinical manifestations. The damage that occurs in the brain and potential complications can be minimized if given an immediate medical intervention.
Ischaemic Stroke:
It is the most commonly occurring cause of stroke. When the interruption of the blood supply is due to a blockage in the blood vessel by a clot or thickening of the artery walls, it is called as an Ischaemic Stroke.
Blood clots typically form in areas where the arteries have been narrowed or blocked by fatty cholesterol-containing deposits known as plaques. There are two types of Ischaemic Stroke viz. Thrombotic Stroke and Embolic Stroke.
A Thrombotic Stroke occurs when a blood clot impairs blood flow in an artery that supplies blood to the brain.
An Embolic Stroke occurs when a blood clot that forms elsewhere in the body (embolus) breaks loose and travels to the brain via the bloodstream. Eventually, the clot lodges in a blood vessel and blocks the flow of blood, causing a stroke.

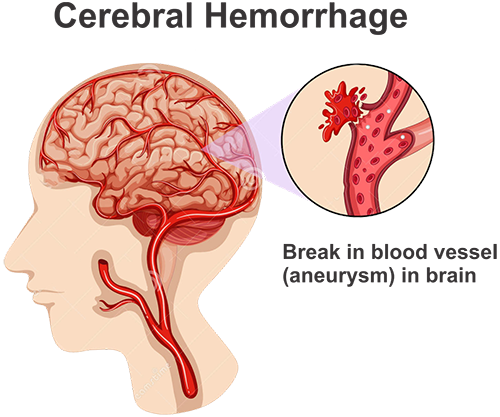
Haemorrhagic Stroke:
This is caused when a weakened blood vessel ruptures, causing it to bleed in the brain. This interrupts with the blood flow leading to a Haemorrhagic Stroke.
There are two types of weakened blood vessels viz., aneurysms and arteriovenous malformations (AVMs).
An aneurysm is a ballooning of a weakened region of a blood vessel. If left untreated, the aneurysm continues to weaken the vessel until it ruptures and bleeds into the brain.
An arteriovenous malformation (AVM) is a cluster of abnormally formed blood vessels. Any one of these vessels can rupture, also causing bleeding into the brain.
Transient Ischaemic Attack (TIA):
When there is a temporary disruption in the flow of the blood supply, it is termed as Transient/temporary Ischaemic Attack. It is also called as a 'mini stroke'. It usually recovers within 24 hours. Like an ischemic stroke, a TIA occurs when a clot or debris blocks blood flow to part of your brain. A TIA doesn't leave lasting symptoms because the blockage is temporary.
It however, still needs immediate intervention, to distinguish it from an actual stroke, and is often also considered as an indicator of the possibility of another stroke.
A stroke is usually considered a lifestyle disorder, wherein, various unhealthy habits cause cardiovascular issues, that increase the risk of stroke. It could also happen due to hereditary disorders.
The more risk factors, the higher the chances of having a stroke. Certain risk factors can be controlled, such as high blood pressure and smoking. Other risk factors, such as gender and age, cannot be controlled.
The major risk factors for stroke include:
High blood pressure
High blood pressure is the highest risk factor for stroke. Blood pressure is considered high if it stays at or above 140/90 mmHg for three consecutive days at the same time, when taken in the same posture. For diabetic or people with chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher.
Diabetes
Diabetes is a disease in which the blood sugar level is high because the body doesn’t make enough insulin or doesn’t use its insulin properly. Insulin is a hormone that helps move blood sugar into cells where it’s used for energy. Prolonged discrepancies of blood sugar can increase the risk of stroke.
Cardiovascular Disease
Any cardiovascular disorder, such as coronary heart disease, cardiomyopathy, heart failure, and atrial fibrillation can cause blood clots that can lead to a stroke.
Smoking
Smoking can damage blood vessels and raise blood pressure. Smoking also may reduce the amount of oxygen that reaches your body’s tissues. Exposure to secondhand smoke also can damage the blood vessels.
Age and gender
The risk of stroke increases with age. However, men are more likely than women to have strokes at younger ages. However, the fatality from a stroke is observed to be higher in women. Women who take birth control pills also are at slightly higher risk of stroke.
Race and ethnicity
Strokes are observed to occur more often in African American, Alaska Native, and American Indian adults than in white, Hispanic, or Asian American adults.
Personal or family history of stroke or TIA
A past history of a stroke increases the chances of another stroke. People with strong family history of strokes also have a higher chance of suffering from one too.
Brain aneurysms or arteriovenous malformations (AVMs)
A balloon-like bulge of tangled faulty arteries and veins that can rupture, is known as aneurysm. They may be present since birth, but often aren’t diagnosed until they rupture.

Other risk factors for stroke, most of which can be controlled, include:
Alcohol and illegal drug use, including cocaine, amphetamines, and other drugs Certain medical conditions, such as sickle cell disease, vasculitis (inflammation of the blood vessels), and bleeding disorders, a sedentary lifestyle, obesity, stress and depression, unhealthy cholesterol levels, an unhealthy diet. The excessive use of nonsteroidal anti-inflammatory drugs (NSAIDs), but not aspirin, may also increase the chances of a stroke, particularly in patients who have had a previous cardiac attacks or cardiac bypass surgery.
The extent of neurological involvement may range from mild motor deficits to gross involvement of various functions, namely, sensorimotor, perceptual, emotional, behavioral, memory intelligence, speech and language function, ultimately affecting daily activities.

The commonly seen symptoms are:
Weakness of the face, arm, or leg on one, or both sides of the body
Imbalance while sitting or standing
Lack of coordination while doing activities (ataxia)
Loss of vision or dimming (like a curtain falling) in one or both eyes
Loss of speech, difficulty in talking, or understanding what others are saying
Sudden, severe headache with no known cause
Problems associated with hearing
Behavioral issues
A brain stroke is a medical emergency and the patient should be taken to a hospital as soon as possible to prevent further damage to the brain. Investigations such as Computed Tomography (CT) Scan help in confirming the type of stroke.
In case of ischemic stroke, it is common to give aspirin to reduce the risk of death or of a second stroke. If the cause of the stroke was a clot, it is possible that the quick administration of certain clot-dissolving drugs, such as tissue plasminogen activator (tPA), may prevent some symptoms such as paralysis. Another option is mechanical removal of clot, which should be performed within six hours of onset of symptoms of stroke.
In case of hemorrhagic stroke the aim is to control bleeding and reduce pressure in brain. Where there is a blockage or rupture in an artery, a surgical intervention may be required to release the pressure in the brain and repair the artery to prevent future stroke.
Once a stroke has permanently damaged the brain, it is difficult to undo the damage. Rehabilitation following a stroke is very important to restore independence in the patient's daily activities. Physiotherapy, occupational therapy, psychological, and speech and language therapy are needed to improve muscle coordination, hand function, speech and cognitive function.
To prevent future episodes of stroke it is important to follow lifestyle modification, diet modification and regular intake of prescribed medicines. Medically, it is recommended to have regular check-ups of heart and vessel function.

Complete recovery is unusual but not impossible and most patients will improve to some extent with the help of a healthy lifestyle, various therapies and emotional support and motivation from the family members.
With the current treatment approaches, be it medical, surgical or rehabilitative, the pathophysiological processes and the resultant damage occurring at the microcellular level cannot be reversed. This calls for newer and more effective treatment approaches to improve not just the consequences of stroke but to repair and restore activities of the damaged neural tissue.
Researchers and scientists are therefore considering regenerative medicine as a potential approach for stroke. cell, with their unique properties of self-multiplication, differentiate into specialized cells and migrate to the affected area, regenerate and repair the affected tissues in stroke.
Recent experimental studies raised the possibility of using mesenchymal cell (MSCs) for stroke therapy. There is increasing evidence that MSCs promote functional recovery in animal models of ischemic stroke.
In specific culture conditions, human MSCs can differentiate into cells that express markers of neuronal progenitor cells and can engraft and migrate along paths that resemble those of neuronal progenitor cells. Furthermore, the mononuclear fraction obtained from the bone marrow contains several cells including cell and their precursors, which can produce large amounts of cytokines and trophic factors that promote blood and oxygen supply, neuroprotection and neuroregeneration in the affected area.
MSCs are eminently suitable for human trials because these cells can be obtained readily from bone marrow under local anesthesia, are easily expanded by culture, and potentially could be delivered to the injured brain tissue without the need for invasive operations. Moreover, the use of patients' own bone marrow cells should prevent the problems of immune rejection.
This had led doctors, researchers and scientists to believe that regenerative medicine has tremendous potential in improving the condition of the people affected with stroke.
The best medical management, newer neuroprotective drugs and extensive rehabilitation, are still not able to give paralyzed patients symptomatic relief from their paralysis. It is for recovery of this that we at NeuroGen are offering regenerative medicine as a new beacon of hope.
With the fervor to do better and bring about positive transformations in the lives of our patients, we at NeuroGen BSI have treated over 200 patients with stroke. Majority of the patients who had approached us, had reached a plateau stage in their symptomatic and functional improvements. However, after regenerative medicine, our patients showed remarkable improvements in several of the symptoms such as upper limb activity/hand functions, lower limb activity, trunk activity, balance, higher mental functions/speech, ambulation and activities of daily living. This gives them a possibility of returning to their daily routine and to maintain their independence.


Our studies illustrated that 51.8% of patients showed significant improvements, 29.6% of patients showed moderate improvements, mild improvements were observed in 11.1% of the patients, promising a future they always deserved.

These improvements are not just restricted to the functional and symptomatic changes that are seen in our patients but also go a step further. The cell administered during the course of the therapy work wonders in repairing the damage in the stroke affected regions of the brain by increasing their metabolism as observed in the PET-CT scans.
Objective Radiological evidence of improvement after regenerative medicine in a case of stroke


PET CT Scan of the brain before Regenerative Medicine show the blue areas that represent reduced brain activity due to the damage that occurs to the brain tissue after stroke.


PET CT Scan of the brain after Regenerative Medicine showing improved metabolism in frontal lobe, occipital lobe, and basal ganglia on the left side as indicated by the circles.
The extent of recovery varies from case to case. A stroke damages the brain cells. The extent of the brain damage and the size of the stroke are directly related to the extent of the impairments/paralysis.
People who suffer a minor stroke may have only slight impairments/problems, such as a weak arm or leg (paraparesis or hemiparesis). A massive stroke, however, can cause a person to lose the ability to read, write, or speak. It also can cause paralysis.
Fortunately, with rehabilitation, such as physiotherapy, occupational therapy, speech therapy, about 25% of stroke patients recover with slight impairments and an additional 10% recover almost completely.
With the addition of regenerative medicine, to the rehabilitation, the extent of improvements can increase.
The type of treatment provided depends on the type and severity of the stroke. If the victim has suffered an ischemic stroke, immediate therapies may include medications to dissolve the clot, surgery, and/or interventional neurosurgery, such as stenting and so on. If the victim has suffered a hemorrhagic stroke, immediate therapies may include medications and/or surgery.
REMEMBER: The sooner the victim receives treatment, the better his or her chances are of survival and recovery.
Rehabilitation is a very important aspect of the recovery process in Stroke survivors. NeuroGen Brain and Spine Institute offer patients the most comprehensive and holistic stroke rehabilitation in Mumbai and India. Our rehabilitation program includes speech therapy, physical therapy, and occupational therapy, with experienced staff that specialize in helping stroke and patients with other neurological disorders regain their independence.
Regenerative Medicine helps repair the damage to the brain and stimulates the parts of brain, which are functioning less (after the brain stroke). It is complementary to the rehabilitation. Regenerative Medicine along with a comprehensive rehabilitation program helps in accelerating the process of recovery.
Cell is not a substitute for rehabilitation; it works hand in hand with the exercises.
At NeuroGen Brain and Spine Institute, the best of neurorehabilitation is combined with the newest technology of regenerative medicine, which makes treatment for stroke patients more effective.
The biological task of cell is to repair and regenerate damaged cells. Regenerative Medicine utilises this function by administering these cells in high concentrations, directly in and around the damaged tissue, where they advance its self-healing and repair.
Bone marrow transplantation has been used successfully for genetic disorders of blood, such as sickle cell anemia, thalassemia, as well as cancers such as leukemia. Since our therapy uses these very cells, which are harvested from the patient's own body (autologous cells), there are no major ethical concerns. Ethical concerns are primarily on the use of embryonic cell (which we do not use).
The therapy is done under local anesthesia and a mild sedation. There is no significant pain or discomfort during or after the procedure.
Regenerative Medicine is minimally invasive and reasonably safe. None of our patients have shown any neurological deterioration so far in connection with regenerative medicine itself. Some short-acting side effects, such as headache (spinal headache) lasting 3-4 days which is generally self limiting, neck/back pain, vomiting, some mild rash or pain at the site of bone marrow aspiration/cell injection may occur. However, like any other medical or surgical treatment unexpected complications are always a possibility. These complications may be related to the medicines given, the cell procedure, the anesthesia, and the rehabilitation or to any of the preexisting medical or neurological conditions.
Maximal improvements are seen around 3-6 months after the treatment. However, in many patients there are slow progressive improvements that continue for several months/years later. Most patients do show some immediate improvements also i.e. before the discharge, in some of their symptoms.
The decision to do the therapy a second time is taken after seeing the progress/improvements after the first therapy. If the patients show some encouraging improvement, then the entire medical and rehabilitation team reviews the case and a second treatment may be recommended. This may be done anytime between 3-6 months of the first therapy.
We will review what other medications the patient is already on. In most cases we do not discontinue any already going on treatment. However, this is decided on a case-by-case basis. Blood thinners like aspirin, clopidogrel, warfarin, etc. need to be stopped. Please inform us about any medications you are taking beforehand.
This is difficult to predict, since each patient varies. It depends on multiple factors such as age of patient, severity of symptoms, duration of illness and extent of rehabilitation taken after the treatment.
At NeuroGen Brain and Spine Institute, we have treated over 200 patients of stroke, with a combination of regenerative medicine along with rehabilitation. All these patients had attained a plateau stage with respect to symptomatic and functional improvements. The symptoms they presented with included upper limb activity/hand functions, lower limb activity, trunk activity, balance, higher mental functions/speech, ambulation and Activities of Daily Living.
Our data is regularly published in various medical and scientific journals (available for reading on our website). You are strongly advised to study these before proceeding with treatment.
Case Report 1
Our patient Mr. CD suffered from stroke only at the age of 19 years. Seven years after suffering the stroke for the first time, he visited NeuroGen. He was primarily affected on the left side of his body. When he came to us, he mainly complained of difficulty in walking, imbalance, abnormal gait, weakness in his left hand, difficulty in using his left upper limb, difficulty in climbing stairs. He used to find it difficult to transfer himself at lower or higher level place. He was experiencing mild depression. When we examined him further, he also had abnormal muscle tone in left upper limb muscles. His movement control was also greatly affected.
At NeuroGen, he underwent Regenerative Medicine along with a customized rehabilitation program. The aim of the rehabilitation program was to develop disassociation and gait training, therapies to increase the strength of the affected areas without fatigue and to increase overall stamina of the patient. He was given exercises that would help him improve his balance, walking, stair climbing, speech, posture and his grip. These exercises were carried out in a systematic pattern with sufficient rest intervals. Together, the aim of the rehabilitation program was to improve his overall quality of life. Mr. CD found new hope with NeuroGen's Neuroregenerative Rehabilitative Therapy (NRRT). He was motivated and optimistic. Physiotherapy, Occupational Therapy and rehabilitation taught at NeuroGen were continued at home.
He came to us after three months for a review. The abnormal muscle tone had reduced. Upper limb overhead activity had improved, shoulder range increased, effort reduced. Upper limb fine motor activity had also improved. He could stand for a longer period of time with a more erect posture. His walking speed had increased, with a much-reduced effort. Balance in standing and walking had improved. He could ascend and descend stairs faster. His left upper limb and ankle movement control was slightly better. He could do upper body dressing faster and with lesser effort. He was very focused and underwent rehabilitation diligently.
Case Report 2
Mrs. LM, a 54 year old female suffered a stroke and had paralyzed her right side of the body. In August 2016 she visited NeuroGen to take treatment for the same. When she came to us, she was completely dependent for all activities of day-to-day living. When we examined her she showed some abnormalities of tone in the muscles. Her speech was unclear. Her voluntary movement was affected. She had profound weakness in the muscles of her right side. She needed two people to assist her in walking.
With the impairment caused by stroke she had pinned a lot of hope in regenerative medicine. She continued vigorous therapy post regenerative medicine. When we saw her three months later, she was a whole new individual. Her walking ability had significantly improved. She could walk independently with a cane (minimal support). Her balance in standing and walking had improved greatly. Her movements of shoulder and elbow were more controlled and faster than before. Her stamina had improved. The tone abnormalities of the muscles had reduced. Her speech had become clearer. Her urine control had improved. Six months after regenerative medicine her improvements was consistent. Furthermore, her walking pattern had improved with an increased shoulder control. The abnormal tone had almost normalized. Balance was better. She started climbing stairs with minimal assistance. Her bladder control had returned. She was minimally dependent for her day-to-day activities and was very eager to be completely independent again. She was very driven and motivated and complied with rehabilitation. Looking at the results from the first regenerative medicine she decided to do it again, and 7 months after the first regenerative medicine she underwent regenerative medicine once again.